Evaluation Of Probe Guide: Software-assisted Probe Tube Placement In Hearing Aid Fittings
By Paula Folkeard, AuD; John Pumford, AuD; Jonathan Pietrobon, MESc, and Susan Scollie, PhD
Feb 13, 2020
A new software-assisted system for placement of the probe tube in real-ear measurement (REM) has been developed by Audioscan. This article describes the new Probe Guide tool and compares its performance with traditional methods for probe tube placement.
Research has highlighted the benefits of conducting real-ear measurements (REM) for both patients and clinicians. Routine verification of aided hearing aid responses using REM is also a part of recommended practice.1,2 Yet, despite professional guidelines, best-practice statements, and research evidence, REM is not routinely performed by clinicians.3,4 In fact, failing to verify hearing aid fittings using probe-microphone measurements has been listed as the number-one mistake made by clinicians.5
While various theories have been proposed, lack of REM use is attributed by some to the perceived complexity of the REM process, including proper positioning of the probe tube in the ear canal.4 The literature generally indicates that the end of the probe tube should be placed within 5 mm of the eardrum (while avoiding contact and any associated discomfort) to obtain accurate measurements, particularly in the high frequencies, given the influence of standing waves along the ear canal.6-10
ANSI S3.46-201311 outlines various methods to obtain proper probe tube placement for REM including: visually assisted positioning using a standard probe tube insertion depth and otoscopy; geometrical positioning leveraging the lateral portion of an existing hearing aid or earmold8, and, two acoustical techniques which use standing waves in the ear canal to assist in probe tube positioning:
1) Acoustically assisted positioning using the stability of the REUR measurement at 4-6 kHz and
2) Acoustical positioning using a continuously presented 6 kHz narrow-band stimulus.
These probe tube placement methods can be used to generate clinically appropriate measurements that have good reliability;7,8,10,12 however, they are arguably not always easy to execute or interpret, depending on the ear canal and experience of the clinician.
Training is commonly provided to develop clinical competency in probe tube placement and can include in-person training, the use of mannequin simulators,13 and software-assisted feedback systems such as the probe tube placement tool described in this paper.
Probe Guide
In an effort to increase the use of REM in clinical practice and to aid clinicians with obtaining proper probe tube insertion depth, Audioscan has developed Probe Guide. This clinically feasible, software-driven, acoustic-based tool was developed using a patent-pending machine-learning algorithm to guide probe tube placement in real time.
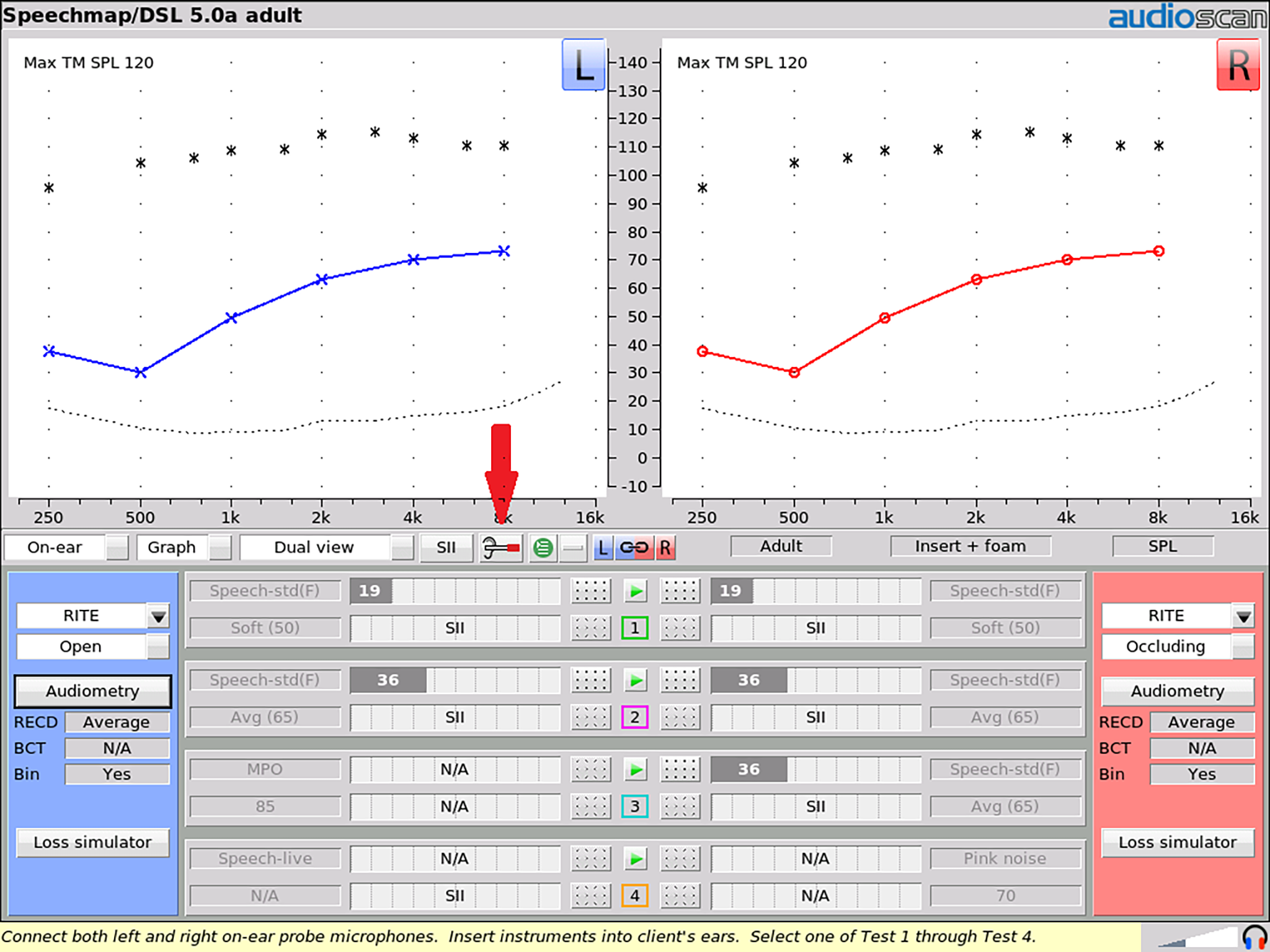
Figure 1. Probe Guide is accessed using the highlighted icon button on any on-ear test screen.
While a broadband noise signal is presented from the REM loudspeakers, the spectrum of sound within the ear canal is repeatedly sampled, analyzed, and input into a model of probe tube depth developed from a previously measured set of in-ear recordings. These recordings were gathered with normal adult ear canals as the probe tube was advanced to the correct location relative to the tympanic membrane.14 The machine-learning algorithm was “trained” to estimate probe tube depth from a sequence of input spectra, resulting in a software system that detects correct probe placement in real time.
A typical next step in machine-learning tool development is to test the trained system on a new dataset to evaluate whether the trained system works on new patients. Therefore, the purpose of the following collaborative study was to validate the performance of Probe Guide on a new set of ears. Our goal was to determine the performance of this new tool by comparing measured probe tube insertion depths between Probe Guide and a clinician-appraised depth, the adequacy of REMs made with Probe Guide, and the presence of any procedural issues (eg, eardrum contact) obtained with Probe Guide (PG) versus an experienced audiologist using a traditional visually assisted (VA) method of probe tube placement.
How to Use Probe Guide
Probe Guide can be accessed on any on-ear test screen on Audioscan Verifit2 (software version 4.18 and later) and Axiom (software version 1.24) by clicking the provided icon button (Figure 1). The guidance in probe tube placement is shown in Steps 1-3 below (Figures 2-4).
STEP 1: Setup
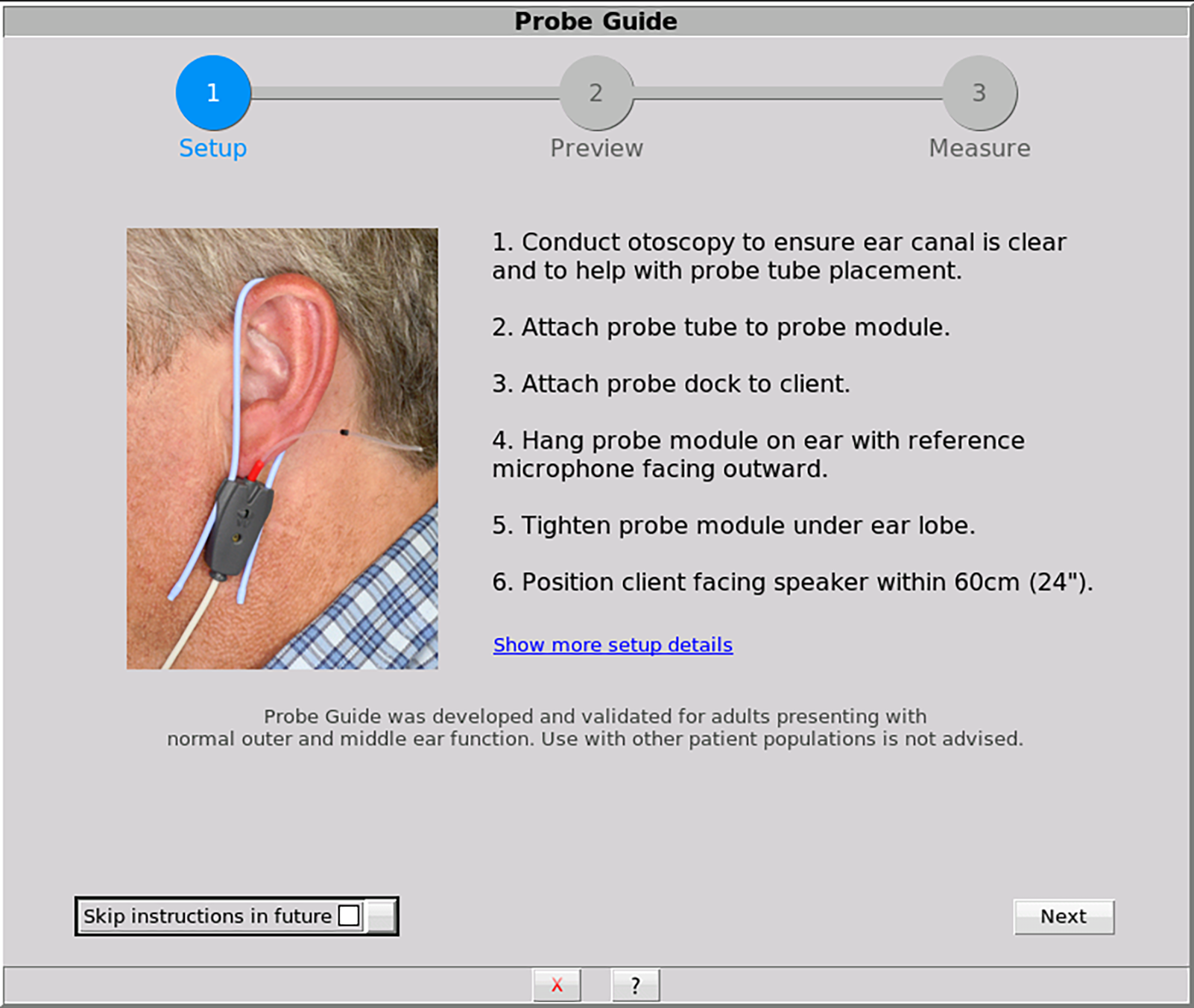
Figure 2. This optional screen describes methods for preparing the client and the equipment for probe tube placement
STEP 2: Preview
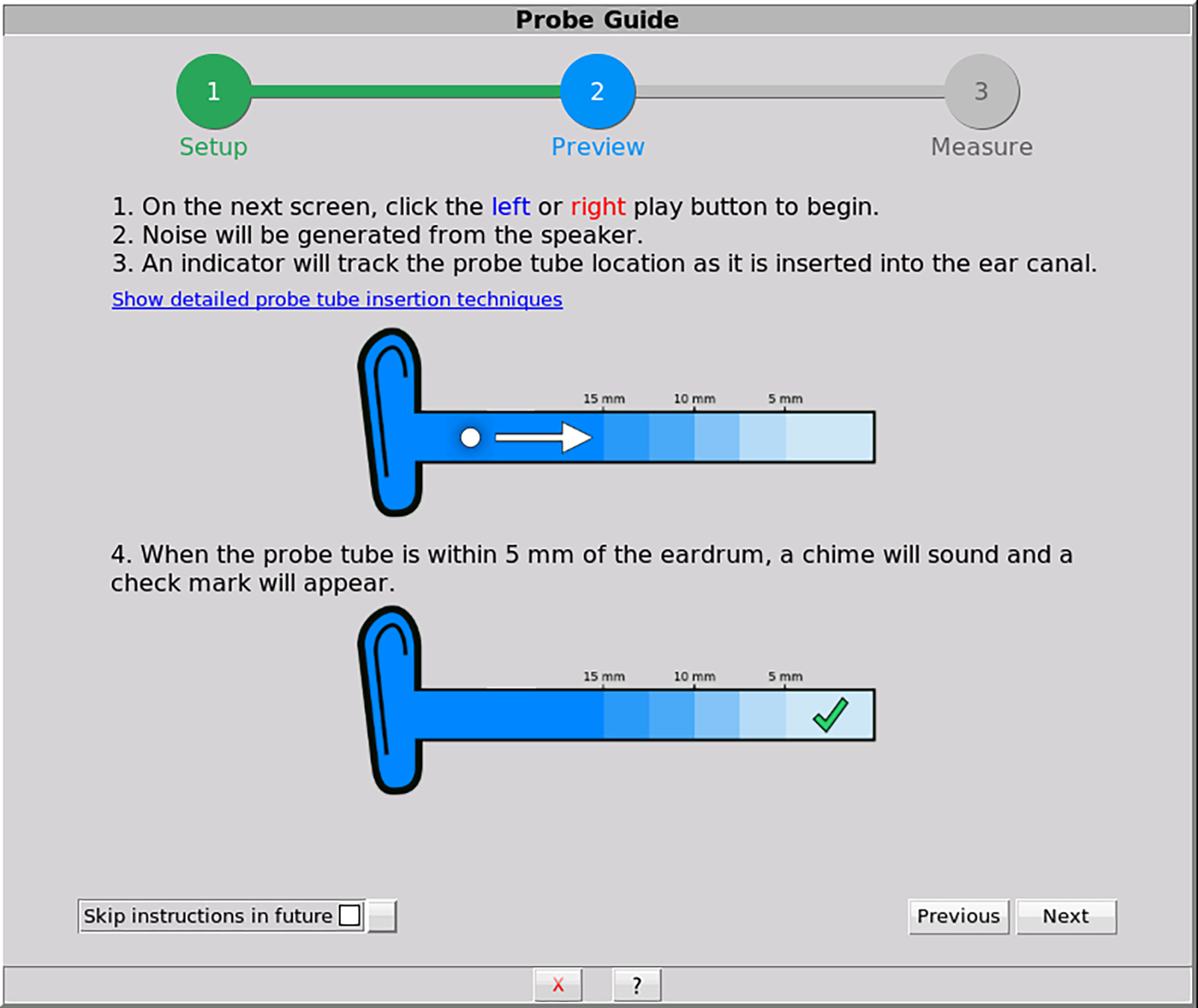
Figure 3. This optional screen describes procedural details on using Probe Guide to support proper use and counseling.
STEP 3: Measure
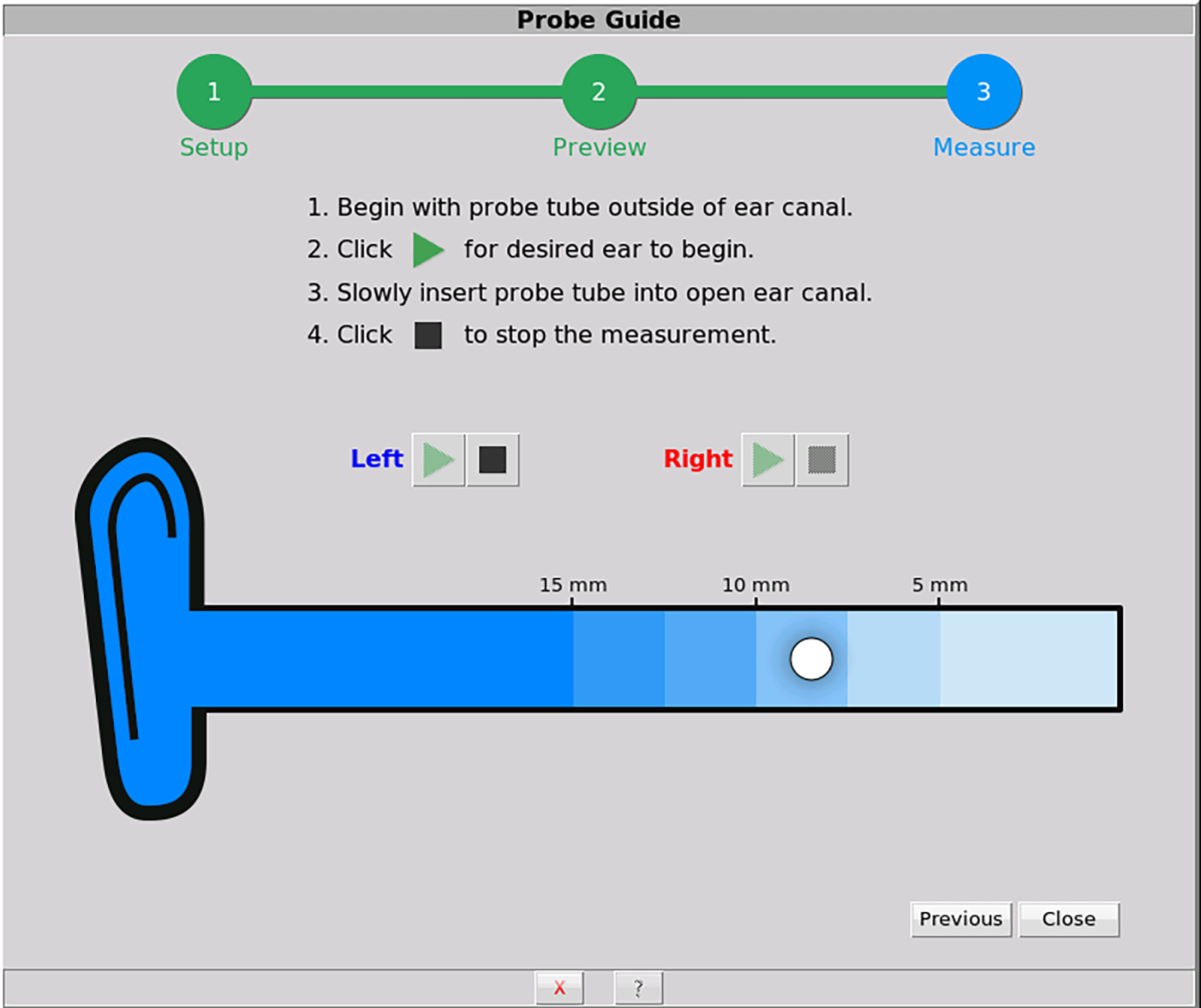
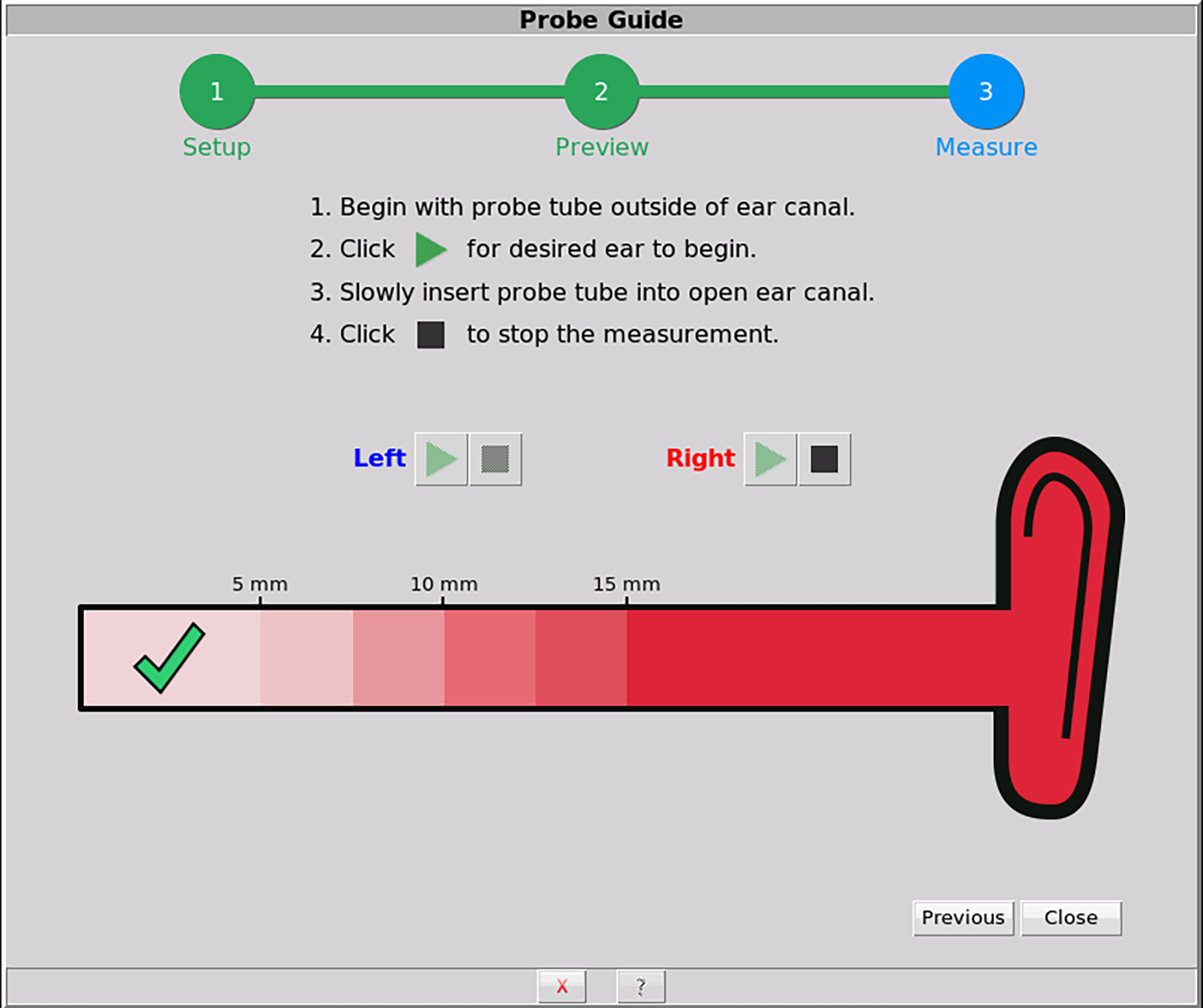
Figures 4a-b. This screen is used when performing the guided probe tube placement. A white ball tracker indicates real-time location of the probe tube. A green check mark and a chime is generated when the probe tube is within 5 mm of the eardrum.
Probe Guide Validation Study
The current study investigated the performance of the software-assisted Probe Guide method as implemented on Verifit2 relative to an expert clinician’s probe tube placement using the traditional visually assisted positioning technique. The expert clinician had more than 20 years of experience placing probe tubes for both clinical and research purposes.
Evaluation measures for each placement method included absolute probe tube insertion depth, test-retest reliability of probe tube insertion depth, real-ear unaided responses (REUR), and the occurrence of any procedural concerns (eg, patient discomfort, visual acceptability of placement, reported eardrum contact). A total of 20 participants (10 males and 10 females, ages 25-81) completed the protocol. All subjects had normal middle ear and external ear canal status as determined by otoscopy and impedance measurements.
Probe tube placement was completed on 40 adult ears, twice using the visually assisted method, and twice using Probe Guide. The starting order was counterbalanced across ears and placement methods. A within-subjects design was used to measure these system performance variables at the individual level. The probe tube marker, typically used to aid with probe tube placement, was moved to the base of the probe tube so as not to influence insertion depth decision-making.
For the visually assisted method, the probe tube was placed considering anatomical markers that correspond to a distance of approximately 5 mm from the tympanic membrane. The clinician used otoscopy to monitor the probe tube location. For the software-assisted method, the probe tube was inserted until Probe Guide indicated the proper insertion depth had been achieved.
Following probe tube placement with either method, the REUR was measured using a 65 dB SPL pink noise following the standard ANSI S3.46-2013 REM procedure. Next, the probe tube was marked with a fine felt tip pen at the intertragal notch. The probe tube was then removed from the ear canal and the distance from the medial end of the probe tube to the marked line was measured to calculate the insertion depth in millimeters. The mark was removed and the procedure was repeated again to evaluate test-retest reliability. The procedure was completed twice in each ear canal resulting in 4 measurements for each participant (Figure 5).
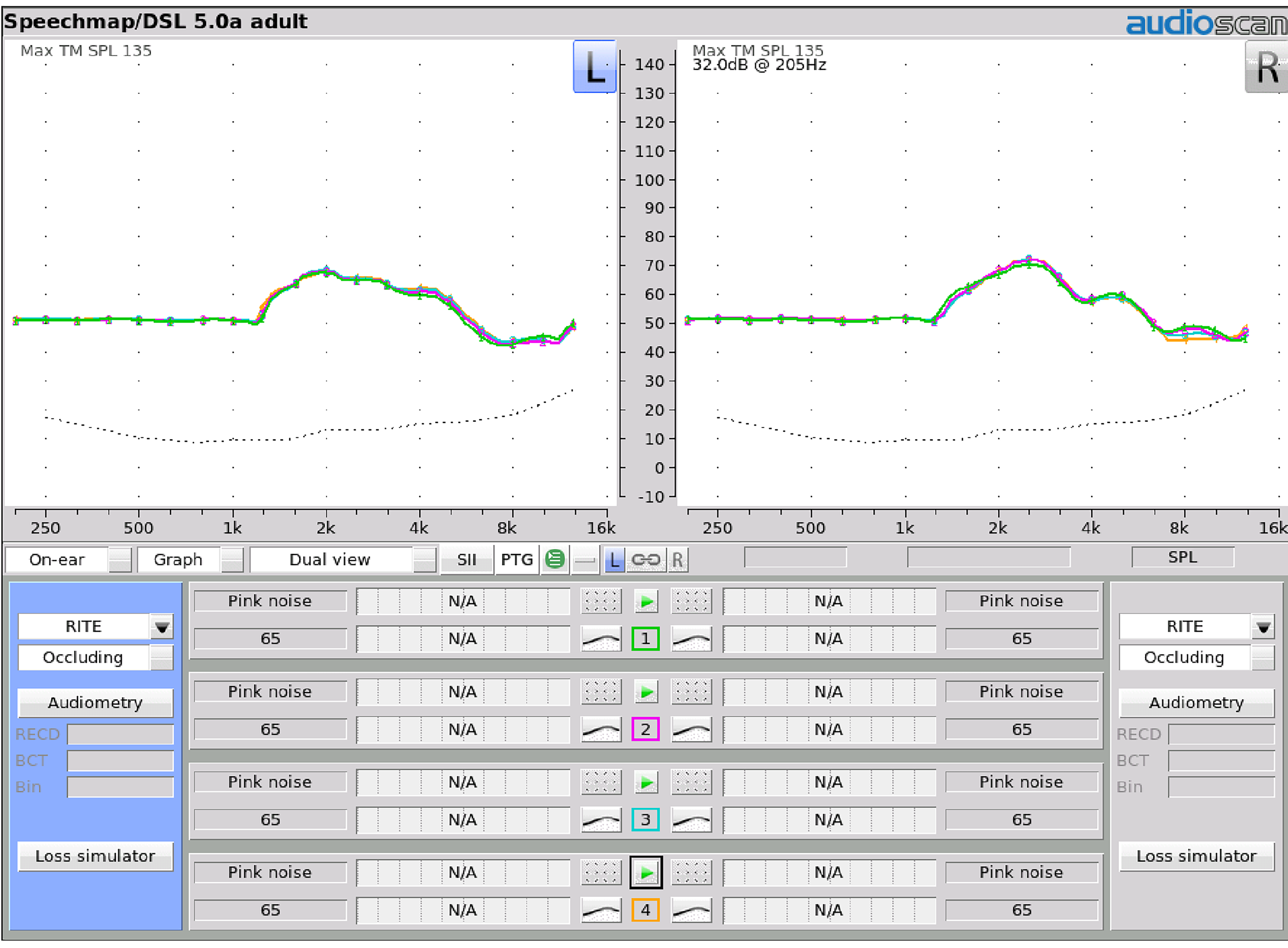
Figure 5. Real-ear unaided response (REUR) measures for one participant. Four REUR measures were completed for each ear. (Test 1 – Visually assisted (VA); Test 2 – VA (second run for test-retest); Test 3 – Probe Guide (PG), and, Test 4 – PG for test-retest).
The Speechmap session files from the Verifit2 were saved and exported in .xml format and imported into a spreadsheet for further analysis. The acoustic differences between the visually assisted and Probe Guide methods were calculated at all 1/12th octave frequencies measured by the Verifit2.
Results
Real-ear unaided response (REUR) measurements.
Group data were analyzed for the 20 participants. All statistics were completed using SPSS v24. A repeated measure analysis of variance (ANOVA) was completed to evaluate differences between probe tube placement methods for: 1) Probe tube insertion depth, and 2) REURs. In addition, within each probe tube placement method, test-retest reliability was evaluated. If significant differences were revealed, post-hoc paired comparisons were completed with Bonferroni corrections.
The ANOVA was completed comparing the results from the two methods, with left and right ears and repetitions as within-subjects measures. Results indicated that frequency was significant (F(6.441, 978.975)=965.712, p=<.001>2 =.864). This result was expected because of the magnitude of the REUR changes across frequencies. Ear tested was not significant (p=.159, η2= .013), meaning results did not change whether we were testing the right or left ear.
For the purposes of this study, we were most interested in the significance of Placement Method. When the four sets of measures (ie, VA, VA-retest, PG, PG-retest) were compared, results indicated that placement method was not significant (p=.966, η2=.002) indicating that the measures within repetitions and between test methods did not differ. The average REUR difference at each frequency is presented in Figure 6 (PG-VA). Descriptively, these results show less than 1.6 dB difference between the visually assisted and Probe Guide measures out to 12,500 Hz. The 95% confidence interval shows that differences between the two placement methods were less than 2.5 dB up to 8,000 Hz, and less than 3 dB up to 12,500 Hz.
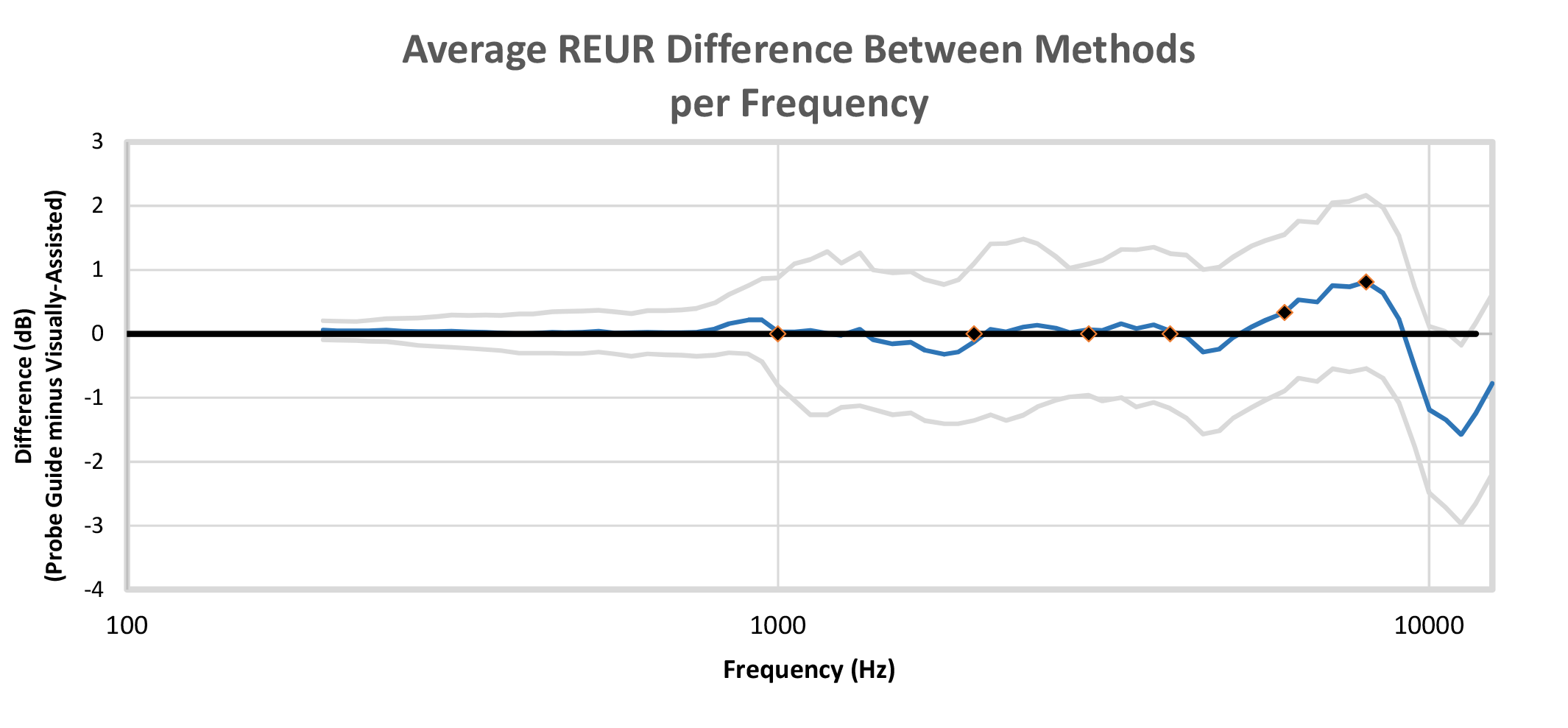
Figure 6. Average real-ear unaided response (REUR) differences across frequencies for a 65 dB SPL pink noise input signal with 95% confidence intervals (PG minus VA). Audiometric frequencies of 1,000-8,000 Hz marked for reference. Results show that, on average, differences were less than 1.5 dB out to 10,000 Hz. The 95% confidence intervals show differences remained below 2.5 dB up to 8,000 Hz and below 3 dB up to 12,500 Hz.
Probe tube insertion depth measurements. Probe tube insertion depths (Figure 7) relative to the intertragal notch for males ranged from 29-41 mm for both placement methods (mean = 33.9 mm using VA; mean = 33.7 mm using PG). For the female group, the probe tube depth ranged from 25.5-34.5 mm (mean = 30.2 mm) using the visually assisted and a range of 25-35 (mean = 30.0 mm) using Probe Guide. As expected, probe tube depth by gender was significantly different (F(1, 0.584)=5995.110, p<.001>2=.345). However, when the probe tube insertion depths for the 40 ears (20 left and 20 right) were compared across the four placement conditions (ie, VA, VA-retest, PG, PG-retest), the ANOVA results indicated Placement Method was not significant (F(2.447, 95.424)=.780, p=.485, η2 =.020), nor was Method by Gender (F(2.467, 93.727)-.669, p=.545., η2=0.017).
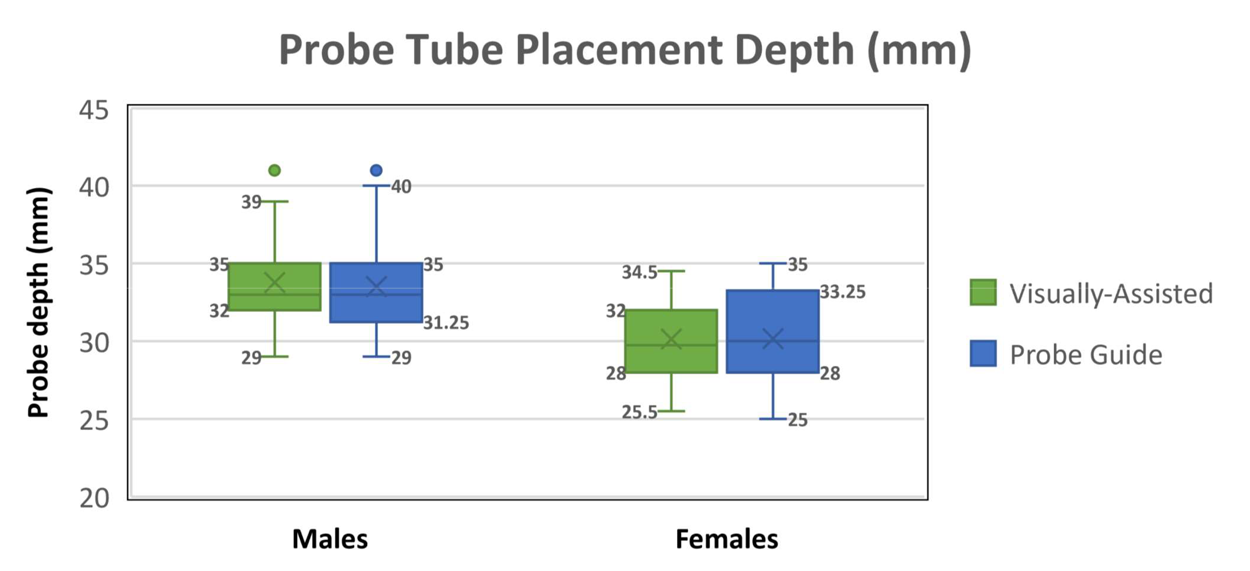
Figure 7. Probe tube insertion depth relative to the intertragal notch for 20 male and 20 female ears. Each box represents the probe tube depth mean (x) median (—); measurement range (I), first quartile (bottom of box), third quartile (top of box), and outliers (•).
Observational reporting of the probe tube placement methods. Of the 160 probe tube placements, there were no reported incidences of contact with the tympanic membrane or discomfort reported using either of the two placement methods. Following each use of Probe Guide, the experienced clinician viewed and commented on the resulting placement. Of the 80 software-assisted Probe Guide placements, one placement was deemed to be too far away from the tympanic membrane (3 mm farther than the visually assisted method) and 5 placements were deemed to be at an appropriate distance but likely too close to the tympanic membrane when inserting a hearing aid or foam tip (2-3 mm closer than the visually assisted method).
Summary
Proper probe tube placement is necessary for valid real-ear measurements, and is therefore an important aspect of verification. In an attempt to assist with this component, Audioscan developed an acoustic-based, software-driven probe tube placement tool called Probe Guide to evaluate the location of the probe tube in the ear canal.
As previous acoustic methods of probe tube placement have been criticized for being time-consuming and complex,15 Probe Guide was designed to be more easily incorporated into the clinical REM workflow. The current study evaluated the accuracy of probe tube placement using this new tool in adult ears with normal outer and middle ear status. Results indicated that Probe Guide provided probe tube insertion depths and resulting REURs that were not significantly different from those obtained by an experienced clinician using the traditional visually assisted probe tube placement method. Test-retest reliability was good for both probe tube placement methods. In addition, Probe Guide resulted in acceptable probe tube placement across the ears evaluated in this study as assessed by an experienced clinician with no reported contact with the tympanic membrane.
It is important to note that this project validated Probe Guide with adults presenting with normal outer and middle ear status, and outcomes with other clinical populations may vary. Further evaluation of this software-assisted probe tube placement tool is required to assess its performance with other patient groups, such as infants, children, and those with atypical outer and middle ear status. In addition, Probe Guide does not preclude the continued use of best-practice clinical protocols for probe tube placement with any patient, including otoscopy.
With these considerations in mind, the positive findings of this study suggest Probe Guide is a useful tool that can assist clinicians with probe tube placement when needed. To the extent that confidence and/or lack of experience with probe tube placement is an obstacle to conducting REM, the results of this study should encourage clinicians to use Probe Guide as a means to more routinely incorporate REM into their practice.

About the authors: Paula Folkeard, AuD, is Research Audiologist/Project Coordinator at Western University’s National Centre for Audiology in London, Ontario. John Pumford, AuD, is Director of Audiology and Education; Jonathan Pietrobon, MESc, is Senior Product Developer at Audioscan in Dorchester, Ontario; and Susan Scollie, PhD, is a Professor at Western University and a researcher at the National Centre for Audiology.
Correspondence can be addressed to Dr Folkeard at: folkeard@nca.uwo.ca
Citation for this article: Folkeard P, Pumford J, Pietrobon J, Scollie S. Evaluation of Probe Guide: Software-assisted probe tube placement in hearing aid fittings. Hearing Review. 2019;26(11).
References
1. Valente M, Abrams H, Benson D, et al [American Academy of Audiology task force]. Guidelines for the Audiologic Management of Adult Hearing Impairment. Audiology Today.2006;18(5):1-44.
2. College of Audiologists and Speech-Language Pathologists of Ontario (CASLPO). Practice Standards for the Provision of Hearing Aid Services by Audiologists. http://www.caslpo.com/sites/default/uploads/files/PS_EN_Practice_Standards_for_the_Provision_of_Hearing_Aid_Services_By_Audiologists.pdf. Published October 18, 2016.
3. Mueller HG, Picou EM. Survey examines popularity of real-ear probe-microphone measures. Hear Jour. 2010; 63(5):27-32.
4. Mueller HG. 20Q: Real-ear probe-microphone measures–30 years of progress? January 12, 2014. Available at: https://www.audiologyonline.com/audiology-ceus/course/20q-real-ear-probe-microphone-23597. Published January 12, 2014.
5. Kochkin S, Beck DL, Christensen LA, et al. MarkeTrak VIII: The impact of the hearing healthcare professional on hearing aid user success. Hearing Review. 2010;17(4):12-34.
6. Dirks D, Kincaid G. Basic acoustic considerations of ear canal: Probe measurements. Ear Hear.1987;8(5):60S.
7. Storey L, Dillon H. Estimating the location of probe microphones relative to the tympanic membrane. J Am Acad Audiol.2001;12:150-154.
8. Bagatto MP, Seewald RC, Scollie SD, Tharpe AM. Evaluation of a probe-tube insertion technique for measuring the real-ear-to-coupler difference (RECD) in young infants. J Am Acad Audiol.2006;17:573-581.
9. Moodie S, Pietrobon J, Rall E, et al. Using the real-ear-to-coupler difference within the American Academy of Audiology pediatric amplification guideline: Protocols for applying and predicting earmold RECDs. J Am Acad Audiol.2016;27(3):264-275.
10. Vaisberg JM, Macpherson EA, Scollie SD. Extended bandwidth real-ear measurement accuracy and repeatability to 10 kHz. Int J Audiol.2016;55(10):580-586.
11. Acoustical Society of America. American National Standard: Methods of Measurement of Real-Ear Performance Characteristics of Hearing Aids, ANSI/ASA S3.46-2013. Melville, NY: Acoustical Society of America; 2013.
12. Sinclair ST, Beauchaine KL, Moodie KS, Feigin JA, Seewald RC, Stelmachowicz PG. Repeatability of a real-ear-to-coupler difference measurement as a function of age. Am J Audiol. 1996;5(3):52–56.
13. Koch RW, Moodie S, Folkeard P, et al. Face and content validity of a probe tube placement training simulator. J Am Acad Audiol.2019;30(3):227-234.
14. Pietrobon J, Pumford J, Folkeard P, McInerney C. Application of real time recurrent neural networks for estimating probe tube insertion depth. Poster presented at: The 2018 International Hearing Aid Research Conference (IHCON); August 15-19, 2018;Lake Tahoe, CA.
15. Searchfield GD, Purdy SC. Probe microphone placement for real ear measurement. Am J Audiol.1997;6(2):49-54.